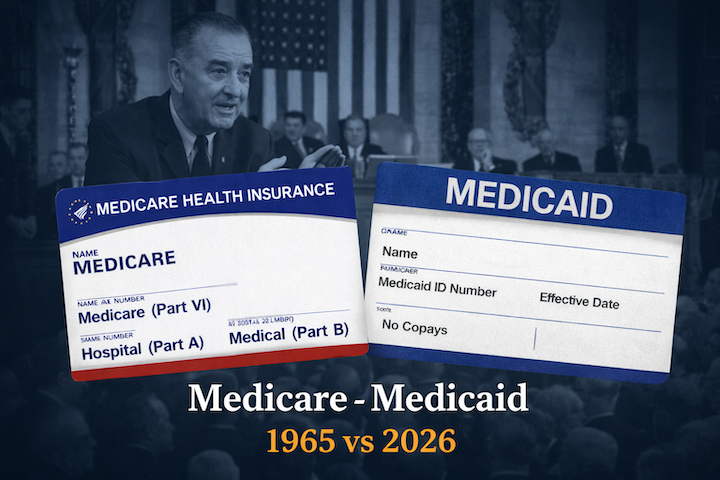
In the summer of 1965, the United States made one of the most consequential social policy decisions in its history. With the signing of the Social Security Amendments, President Lyndon B. Johnson created two landmark programs: Medicare and Medicaid.
They were designed to solve two different crises:
- Medicare — Health insurance for Americans age 65+ and later for certain people with disabilities
- Medicaid — Health coverage for Americans with limited income and resources
Together, they reshaped how Americans age, how hospitals operate, and how the federal government finances health care.
BEFORE MEDICARE: WHAT HAPPENED WHEN SENIORS GOT SICK?
Before 1966, growing old often meant losing access to health insurance.
Most seniors relied on:
- Personal savings
- Financial support from children
- Charity hospitals
- Delaying or skipping treatment
Private insurance companies either refused coverage or charged extremely high premiums to older adults because age meant higher medical risk.
Serious illness could wipe out a lifetime of savings in months. Many elderly Americans entered poverty because of medical bills. This was the central problem Medicare was created to fix.
WHY MEDICARE WAS CREATED
Medicare had two core goals:
- Guarantee hospital and medical insurance for seniors
- Protect retirees from financial ruin due to illness
It was not designed as welfare. Medicare functions more like social insurance, funded through payroll taxes paid during working years.
Medicaid, on the other hand, was designed as a means-tested safety net for people with low income, including children, pregnant women, people with disabilities, and eventually low-income seniors needing long-term care.
TIMELINE: MEDICARE & MEDICAID HISTORY
1965
Medicare and Medicaid signed into law.
1966
Medicare coverage begins. Over 19 million Americans enroll in the first year.
1972
Medicare expands to include:
- People under 65 with long-term disabilities
- Patients with End-Stage Renal Disease (ESRD)
1983
Hospital payment reform begins. Medicare moves to fixed payments per diagnosis (DRGs) instead of open-ended billing.
1997
The Balanced Budget Act creates Medicare Part C, later called Medicare Advantage, signed by President Bill Clinton. Purpose: use private insurance plans to manage care and reduce costs.
2003
Medicare Part D (prescription drug coverage) established.
2010s
Major investments in fraud detection technology and payment oversight.
2020s
Increased use of prior authorization, data analytics, and tighter billing rules to control fraud and spending.
MEDICARE COSTS: 1966 vs. 2026
| Year | Standard Medicare Part B Monthly Premium |
|---|---|
| 1966 | $3.00 |
| 2026 | $202.90 |
Hospital deductibles and other out-of-pocket costs have risen similarly over time due to medical inflation, longer lifespans, and more advanced — but expensive — treatments.
MEDICARE ADVANTAGE: BENEFIT OR RESTRICTION?
Medicare Advantage was introduced to:
- Offer more plan choices
- Use private insurers to manage costs
- Add extra benefits (vision, dental, drug coverage)
Benefits
- Out-of-pocket spending cap
- Bundled benefits
- Coordinated care in some plans
Tradeoffs
- Limited provider networks
- Prior authorization requirements
- Possible delays or denials for services
Some patients appreciate lower upfront costs and extra benefits. Others prefer Original Medicare’s broader provider access without network restrictions.
HOW FRAUD ENTERED THE SYSTEM
Large national programs with complex billing rules create opportunities for abuse.
Common fraud methods include:
- Billing for services never provided
- Unnecessary medical treatments
- Fake home health services
- Durable medical equipment scams
- Identity theft of patients and doctors
- Kickbacks for patient referrals
Fraud drains billions from Medicare and Medicaid annually.
MAJOR CONVICTED FRAUD CASES
Dr. Farid Fata (Michigan): Administered medically unnecessary chemotherapy and cancer treatments to patients in order to bill Medicare and private insurers.
Convicted/Sentenced: 2015 — Sentenced to 45 years in federal prison
Dr. Jacques Roy (Texas): Directed one of the largest home health care fraud schemes in U.S. history, certifying patients for services they did not need.
Convicted/Sentenced: 2017 — Sentenced to 35 years in federal prison and ordered to pay over $268 million in restitution
Dr. Salomon Melgen (Florida): Performed excessive and unnecessary eye treatments and billed Medicare for unwarranted procedures.
Convicted: 2017
Sentenced: 2018 — Sentenced to 17 years in federal prison
Operation Gold Rush (National DME Fraud Scheme): A large-scale criminal network used stolen Medicare beneficiary and physician identities to submit fraudulent durable medical equipment (DME) claims worth billions.
Major Federal Crackdown Announced: 2024–2025
Multiple defendants across states have been charged and convicted as part of the operation, with ongoing prosecutions tied to what authorities described as one of the largest health care fraud takedowns in U.S. history.
GOVERNMENT RESPONSE: STOPPING FRAUD VS. ACCESS TO CARE
To combat fraud, the government has:
- Introduced predictive billing analytics
- Increased audits and investigations
- Expanded prior authorization requirements
- Tightened enrollment rules for providers
- Tested pre-approval systems even in Traditional Medicare
While these steps reduce fraud, they also:
- Increase paperwork
- Delay approvals
- Lead to more denials that must be appealed
This creates a difficult balance between protecting taxpayer funds and ensuring seniors receive timely care.
THE BIG PICTURE
Medicare and Medicaid remain two of the most important safety nets in America. They:
✔ Reduced senior poverty
✔ Increased access to hospitals and doctors
✔ Extended life expectancy
✔ Stabilized the health system
But today they also face:
⚠ Rising costs
⚠ Fraud and abuse
⚠ Administrative complexity
⚠ Tension between cost control and patient access
Understanding this history helps seniors make better decisions — and recognize why modern Medicare sometimes feels very different from the program that began in 1966.
-Lê Nguyên Vũ-
Sources for Further Reading
• U.S. National Archives — Medicare & Medicaid Act of 1965
https://www.archives.gov/milestone-documents/medicare-and-medicaid-act
• Centers for Medicare & Medicaid Services (CMS) History
https://www.cms.gov/about-cms/who-we-are/history
• Social Security Administration — Medicare Premium History
https://www.ssa.gov/history
• Kaiser Family Foundation (KFF) — Medicare Advantage & Prior Authorization
https://www.kff.org/medicare
• HHS Office of Inspector General — Medicare Advantage Denials Report
https://oig.hhs.gov
• U.S. Government Accountability Office (GAO) — Improper Payments Reports
https://www.gao.gov
• U.S. Department of Justice — Health Care Fraud Cases
https://www.justice.gov/criminal-fraud/health-care-fraud-unit
